Why Turbinate, Adenoid, and Tonsil Surgery Should Be a Last Resort, Not the First
One of the most important elements of healthy, functional breathing is the ability to breathe comfortably through the nose. Yet for many people, nasal congestion and airway obstruction make this seem impossible. Desperate for relief, many turn to surgery: turbinate reductions, adenoidectomies, tonsillectomies, and more. But before taking the surgical route, it is essential to understand the full picture, including the risks, limitations, and the alternatives.
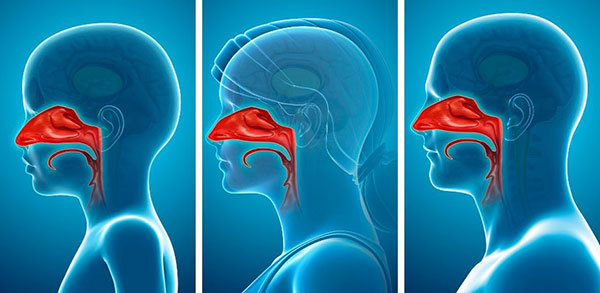
The role of the nose and the danger of underrating it
Your nose is not just a hole to move air. It’s a highly specialized organ with critical roles: warming, humidifying, filtering, disinfecting and regulating resistance to airflow. Structures like the turbinates, tonsils, and adenoids are not just “excess tissue”, they are a vital part of your immune system and your first line of defence against respiratory infections.
Yet, for decades, the common medical approach has been to reduce or remove this tissue when they appear enlarged or obstructive. ENT surgeons often advise that surgery is the only option for chronic congestion or snoring. But this mindset overlooks a crucial fact:
Tissue removal is irreversible. The consequences can be long-lasting, and in some cases, devastating.
The truth about turbinates - Dr. Howard Stupak’s perspective
In his article “The Truth About Turbinates,” Dr. Howard Stupak, a respected otolaryngologist and head and neck surgeon, emphasizes that turbinates are not the enemy and that their function is grossly misunderstood.
Turbinates help regulate the flow, pressure, temperature, and humidity of the air you breathe. Surgically reducing or removing them might create more physical space in the nose, but it disrupts this critical regulatory function. In fact, this can sometimes make breathing feel worse, not better, even when the nose looks "clear" on examination.
“If you remove too much tissue, it can permanently alter the way air flows through the nose,” writes Dr. Stupak. “The turbinates aren’t the problem. Breathing is the problem.”
When surgery backfires: empty nose syndrome
A chilling example of what can go wrong is Empty Nose Syndrome (ENS) a rare but deeply distressing condition where people feel like they can’t breathe, even though their nasal passages are wide open.
The HuffPost article “When a Routine Nose Job Goes Terribly Wrong” documents the experience of several ENS sufferers. Their stories follow a pattern: a surgery intended to relieve congestion leads to a strange, suffocating sensation, chronic dryness, air hunger, and in some cases, depression or suicidal thoughts.
Despite open nasal passages, the brain doesn’t register airflow properly without the turbinates’ sensory feedback. The result is a terrifying paradox: a clear nose, but a constant sense of not getting enough air.
Empty Nose Syndrome (ENS) is a devastating problem caused by the over-resection of the inferior turbinates and/or middle turbinates of the nose. The turbinates are structures in the nose that dilate and/or contract to control humidity, temperature, and filter air that is transported to the lungs.
Read more here »
Surgery is not a shortcut, it’s a final option
The idea that surgery is a quick fix for congestion is oversimplifying the problem. In fact:
- Soft tissues like turbinates and adenoids can regrow, requiring follow-up surgeries.
- Surgery does not address the underlying causes of chronic nasal congestion, like inflammation, allergies, breathing dysfunction, or dietary triggers.
- Many people are never offered less invasive options before being put on the surgical path.
Trimming turbinates or adenoids is like mowing the lawn, the tissue often returns. And once the nasal feedback mechanisms are damaged, recovery is not guaranteed.
Breathing retraining: The least-invasive, most-effective first step
At the Buteyko Breathing Clinic, I’ve spent over 25 years helping people breathe more freely, without surgery. One of the consistent goals in my work is to stress that the least-invasive option should always come first.
Breathing retraining can:
- Improve nasal airflow by reducing inflammation and restoring the CO₂ balance
- Encourage natural decongestion through correct breathing patterns
- Enhance diaphragm use and reduce mouth breathing (which contributes to congestion)
Often, after just a few weeks of breathing retraining and dietary adjustments, clients report significant relief from nasal blockage, snoring, or sleep-disordered breathing, without any need for surgery.
Additional considerations for children and teens may include assessment for tongue tie, Orofacial myofunctional or early intervention orthodontic assessment.
Dr Nic Anderson and his team at Alpers Dental and Dr Alfonso Vargas at Greenlane Dental offer early orthodontic assessments. We work closely with these practitioners and can help assess the suitability and if necessary, the timing for these interventions.
In some cases, surgical intervention may eventually be necessary, particularly cases where nasal obstruction involves cartilage or bone, such as a deviated septum. However, surgery should never be the first option, and it should never be pursued without attempting comprehensive, non-invasive alternatives first.
If you are being advised to undergo turbinate reduction, adenoidectomy, or tonsillectomy:
- Ask your surgeon or GP about long-term outcomes, not just short-term relief.
- Request a referral to a breathing educator such as a Buteyko Institute practitioner.
- Investigate inflammatory contributors: over-breathing, mouth breathing, and stressors such as inflammatory diet, home or work-related stress
- Be aware that functional breathing, not just structural clearance, is the key to nasal comfort.
The goal is not just a "clear" nose, but a functional, comfortable, healthy one. And that begins with breathing well, not short-term symptomatic relief from nasal decongestants, steroids, antihistamines, nasal strips or surgery.
“Remember: always try to breathe through your nostrils, and not through your mouth, because air must contact olfactory nerves to stimulate your brain and put it into its natural rhythm. If you don’t breathe through your nose, in a sense you’re only half alive.”
Robert C. Fulford, D.O.
For more information
For any questions about booking an assessment, breathing retraining or our services contact the clinic on info@buteykobreathing.nz or +64-9-360 6291
View PDF
Posted: Thu 07 Aug 2025
Back
View News index » |
|